Surgeon Spotlight: How Robotics Transformed the Care of a Stroke Patient
- October 18, 2023
- Posted in Surgeon Spotlights
The Surgeon
Dr. Michael D. Fromke is a neurosurgeon affiliated with Lee Memorial Hospital in Fort Myers, Florida. He is transforming the landscape of neurosurgery by utilizing robotic navigation for cerebral hemorrhage evacuation.

The Patient
In June 2023, Dr. Fromke treated a 70-year-old woman who had previously suffered two strokes attributed to atrial fibrillation, one of which left her blind in her right eye. To manage her condition, she had a mechanical mitral valve implanted in 1999, necessitating anticoagulation therapy with Coumadin to maintain an international normalized ratio (INR) of 3.0.
The patient’s condition took a sudden and alarming turn when she presented to the emergency room with rapidly progressing right-sided weakness. Her right upper extremity (RUE) exhibited 3/5 strength, while her right lower extremity (RLE) showed even more severe weakness at 2/5. Loss of sensation in both her RUE and RLE, along with a pronounced loss of fine motor skills in her right hand and apraxia, made her situation dire. Initial assessment indicated a Glasgow coma scale score of 13 (3/6/4) and an intracerebral hemorrhage (ICH) score of 0. Her INR level at admission was 3.17.
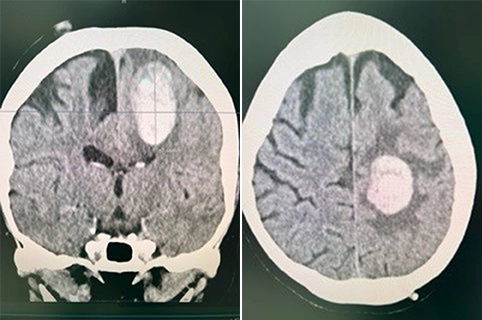
Initial CT scans painted a troubling picture: the patient had suffered an ICH or hemorrhagic stroke. The hemorrhage had occurred in the dominant left parasagittal parietal lobe, with a volume measuring 20ml. The patient evidently required immediate attention and intervention.
The first task was to reverse the effects of Coumadin to ensure the patient’s safety and stability. While the initial ICH had not grown in size on a repeat CT scan, the patient’s neurological symptoms were progressing. Meanwhile, her cardiology team was apprehensive about the risks to her mechanical mitral valve and the possibility of further catastrophic strokes without anticoagulation.
The Challenge
The clinical team was confronted with a complex dilemma. On one hand, the patient required anticoagulation to prevent complications related to her mechanical mitral valve. On the other hand, her hemorrhagic stroke mandated urgent management. The delicate balance between the risk of hemorrhage expansion and the need for anticoagulation was a formidable challenge.
Dr. Fromke opted for a unique strategy. He aimed to stabilize the patient’s neurological status, preserving the vulnerable penumbra surrounding the ICH, while also preparing to resume anticoagulation promptly to mitigate the risk of embolic stroke and mitral valve complications.
Dr. Fromke decided to proceed with robotic-assisted cranial surgery. He reported that “having previously performed a robotic-assisted stereotactic biopsy of a brain tumor in August 2022, I felt comfortable adapting that workflow for this clinical scenario.”

The Robotic Solution
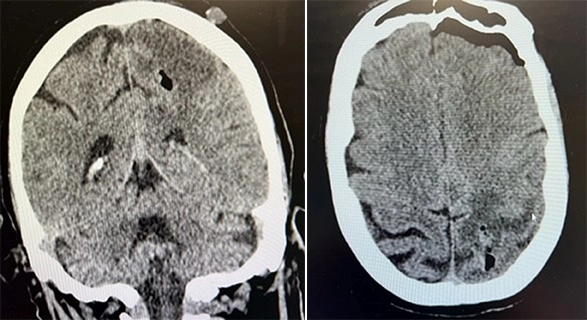
Enter ExcelsiusGPS®. This advanced robotic navigation allowed Dr. Fromke to evacuate the hematoma under control, and there was no active or acute bleeding. Dr. Fromke stated, “The ExcelsiusGPS® robot, along with Excelsius3D® imaging, afforded us with a minimally invasive technique to safely evacuate the hematoma under controlled conditions using a 2.3mm biopsy needle, robot-assisted cranial navigation, and suction control.”

“The ExcelsiusGPS® robot, along with Excelsius3D® imaging, afforded us with a minimally invasive technique to safely evacuate the hematoma under controlled conditions using a 2.3mm biopsy needle, robot-assisted cranial navigation, and suction control.”
– Dr. Fromke
Postoperative CT imaging confirmed the success of the procedure.
The Recovery
Following the surgery, the patient exhibited an astonishing recovery. She regained near complete motor and sensory function in her left arm and leg, along with fine motor skills. Incredibly, she reported being able to write her signature just a few hours after the surgery. The next morning, she was ambulatory without assistance during her physical and occupational therapy sessions. Her mental clarity remained intact, without any signs of lethargy or confusion.
Anticoagulation therapy was cautiously resumed 24 hours post-op. The medical team planned to transition to oral anticoagulation after 72 hours, ensuring the patient’s cardiac health while safeguarding against future embolic stroke events.
The Conclusion
ExcelsiusGPS®, in tandem with Excelsius3D®, proved to be a game changer for Dr. Fromke in neurosurgical intervention, enabling controlled and minimally invasive hematoma evacuation.
Dr. Fromke stated, “Many colleagues perceive emerging robotic technology in neurosurgery to be a fad or gimmick. The real value proposition here is not a specific application of this technology; rather, it is realizing the power of ExcelsiusGPS® as a platform to leverage clinical data and analytics with robotics to drive meaningful innovation to more segments of our patient population and to help improve the overall health of our communities.”
“Many colleagues perceive emerging robotic technology in neurosurgery to be a fad or gimmick. The real value proposition here is not a specific application of this technology; rather, it is realizing the power of ExcelsiusGPS® as a platform to leverage clinical data and analytics with robotics to drive meaningful innovation to more segments of our patient population and to help improve the overall health of our communities.”
– Dr. Fromke
The adaptation of existing robotic workflows, as demonstrated in this case, showcases the versatility of advanced medical technology. The integration of robotics into neurosurgery goes beyond novelty: it is a transformative tool that harnesses integrated planning, navigation, and robotic trajectory alignment for procedural consistency, to ultimately enhance patient care.
